Value-Based Care and Its Global Applications
Value-based care is a healthcare delivery model that incentivizes providers based on improved quality of patient health outcomes rather than solely the quantity of patients served. Proponents of value-based care argue that the approach has many benefits that impact various stakeholders, including patients, providers, payers, suppliers, and society (Figure 1).
Figure 1: Potential stakeholder benefits of value-based care
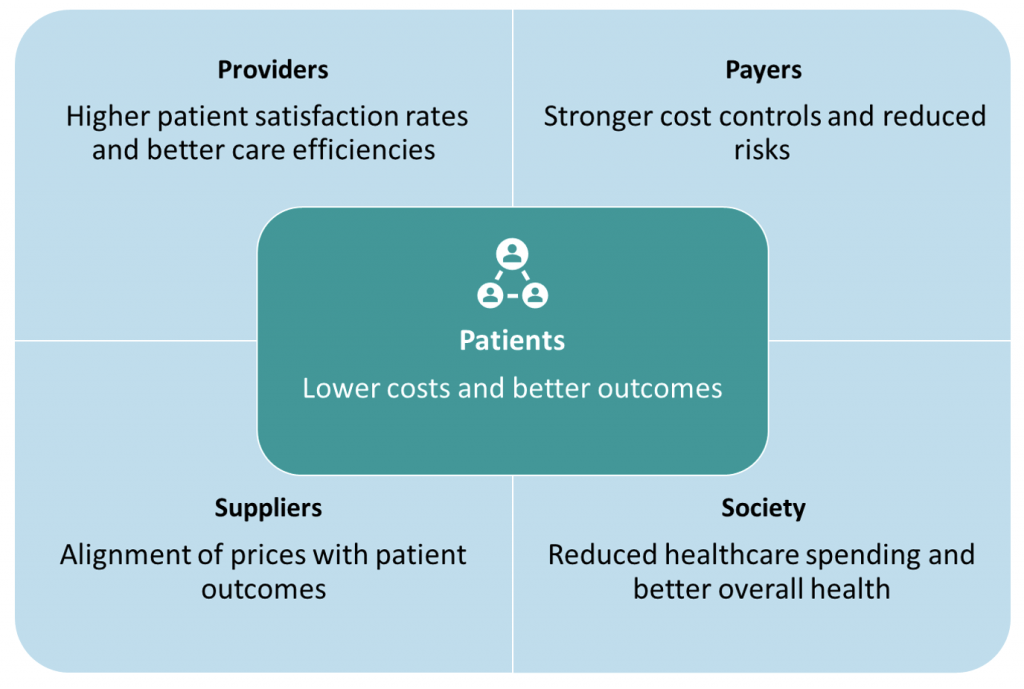
Source: NEJM Catalyst
A growing number of health organizations are moving towards value-based care. Figure 2 shows that, among the G7 countries in 2021, the United States spent most on healthcare, whether measured in dollars per capita or percentage of GDP (17.8%), but has the lowest life expectancy, at 74.2 years. In contrast, Italy and Japan dedicated the lowest amount of per capita spending and percentages of their GDPs (9.45% and 11.13%, respectively) to healthcare but had higher life expectancies.
Figure 2: Life Expectancy and Health Spending, G7 Countries, 2021
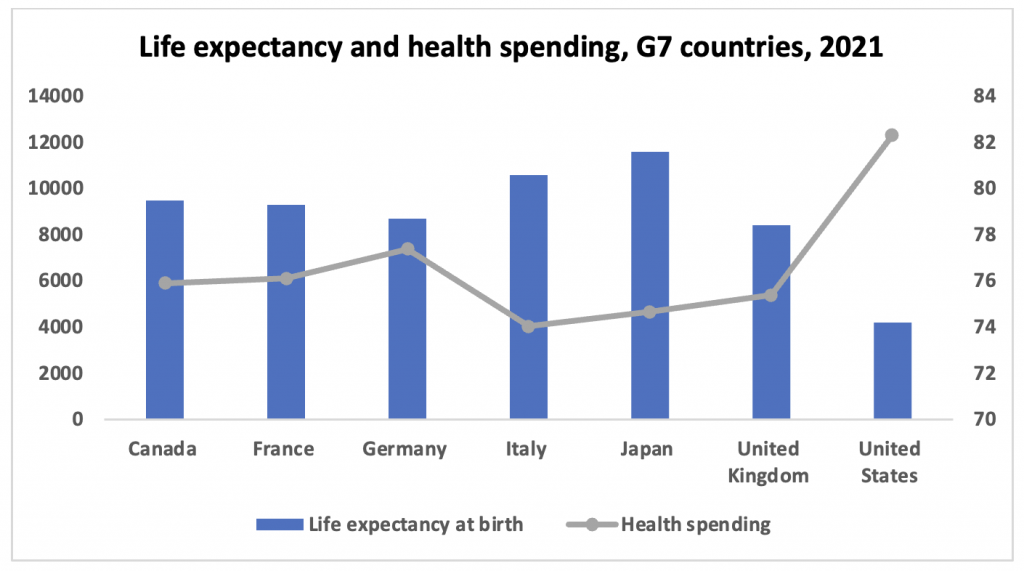
Notes: Health spending (US dollars/per capita), life expectancy at birth (years).
Source: OECD
All G7 countries have implemented some value-based care models but with varying success, due mainly to their type of health system. In some countries, the fragmentation of those systems can present challenges. For example, in France and Italy, value-based care is led by individual institutions.In France, some value-based initiatives have been implemented by the Statutory Health Insurance and the National Health Authority. Not all aspects of value-based care are covered, and the approach has not been as formal compared to the United Kingdom’s National Health System (NHS) Right Care program, a nation-wide project that seeks to reduce unwarranted variations in health outcomes across the country.
To accelerate the adoption of value-based care across health systems, the World Economic Forum developed a framework that describes the main components of value-based care. The framework has been adopted by various jurisdictions and includes the following components:
- Metrics: Since outcomes and costs are at the center of value-based care, it is becoming increasingly important to identify and define measurable outcomes and how they can be reasonably quantified.
- Tools: Various tools (for example, the Healthcare Effectiveness Data and Information Set and the NHS Outcomes Framework) could be used to capture data, at varying levels of the health system (for example, provider, organizational, and regional), that are indicative of quality care and health outcomes.
- Incentives: Some jurisdictions have tied government healthcare funding to specific health outcomes.
Risks of Implementing Value-Based Care
Along with its potential benefits, value-based care is also associated with various potential risks. Experience with implementing value-based care has shown that, since incentives are based on positive outcomes, there is some risk that providers
- only include patients who are already healthy, so they achieve their target outcomes; and/or
- adjust risk scores to make members appear sicker than they are, to gain a greater fee per enrollee.
The first situation occurs when policies incentivize achieving healthy outcomes without considering the baseline of the patient. As such, providers could be expected to opt for accepting patients who would be less costly for them, but who could also support them in achieving their targets.
To address this issue, the United States follows a risk-adjustment approach in which insurers are paid more for patients who will likely require a higher level of care. This approach could have disincentivized providers from avoiding sicker and more costly patients. The risk-adjustment approach has resulted, however, in the second situation described above: providers fraudulently adjusting risk scores to receive bigger payments from the government.The Medicare Payment Advisory Commission estimated that in 2020, the risk scores for beneficiaries in the United States’ Medicare Advantage Plans were about 9.5% higher than what they should have been, resulting in roughly $12 billion in excess payments to plans.
One way to mitigate fraudulent incidents is to adopt artificial intelligence-based tools that could scour patient records for details that could substantiate patient risk scores.As this trend becomes more mainstream, it could likely become a requirement.
Given these potential problems with value-based care, investors may choose to be wary about how managed care companies are adjusting risks and whether fraudulent incidents are likely to occur for a given company, as well as how health outcomes are being measured.
Focus on the United States
As noted above, the U.S. spends the most money per capita on healthcare of any G7 country yet has the lowest life expectancy among G7 countries. The U.S. government is therefore implementing innovative approaches to help contain the health costs of Medicare and Medicaid beneficiaries. For example, the Centers for Medicare & Medicaid Services (CMS) provide policy guidance and support to encourage value-based care and quality across different U.S. states. Through the Medicaid Innovation Accelerator Program (IAP), the CMS works with states to support system-wide payment reform and innovation in delivery systems.
The CMS uses a risk-based contracting approach to increase budget predictability, contain Medicaid spending, and improve value and access to care. This is achieved through “withhold” or “incentive” arrangements between state Medicaid agencies and managed care companies, in which payments are either withheld or increased based on quality metrics and value-based payment (VBP) targets. This arrangement suggests that a certain percentage of funding is at risk should certain targets not be met. This percentage can vary across states; for example, in 2019, Arizona and Louisiana had 1% and 2% of their funding at risk, respectively.
While VBP targets are decided upon at the state level, quality metrics are outlined in the Healthcare Effectiveness Data and Information Set (HEDIS). This tool, which was published by the U.S. National Committee for Quality Assurance, includes more than 90 measures across 6 domains of care: effectiveness of care, access/availability of care, experience of care, utilization and risk-adjusted utilization, health plan descriptive information, and measures reported using electronic clinical data systems.
In the U.S., the risks of cherry-picking and fraudulently adjusting patient risk scores have led the CMS to develop a toolkit focused on improving monitoring and enhancing oversight. The toolkit aims to assist states in complying with various managed care standards and regulations.
Patient Health Outcomes Are Financially Material
For managed care companies, the benefits of implementing value-based care may outweigh the risks. In fact, government contracts and available funding in some jurisdictions are based on value-based care performance.
Standards authorities, such as the Sustainability Accounting Standards Board (SASB), highlight that improved health outcomes are financially material for managed care companies due to their link to reimbursement rates and bonus payments. SASB suggests that managed care companies that can “improve the health of enrollees may be better positioned to protect shareholder value.”
Managed care companies are expected to address the following five domains outlined in the SASB standards:
- Diet and nutrition
- Exercise
- Stress management
- Mental health
- Smoking or alcohol cessation
Beyond these five domains, additional SASB standards address total coverage for preventive health services.
Measuring Health Outcomes Performance in ESG Ratings
ISS ESG considers key aspects of value in care delivery, with a focus on indicators such as the monitoring and steering of health outcomes. Companies that are performing relatively well on these key aspects of value-based care are those that monitor:
- Performance data (e.g., HEDIS)
- Quality of services by providers
- Patient satisfaction
Performance data includes health outcomes in various categories and for all relevant levels (e.g., physician or group level). For example, group-level performance data could include hospital re-admissions, patient complications, and patient length of stay. Beyond monitoring these indicators, favorable company performance requires a plan to improve performance based on these data. The ISS ESG Corporate Rating considers whether companies have action plans and processes for continuously improving health outcomes.
Companies that monitor quality of services at the provider level can ensure that quality and ethics guidelines are followed in delivery of care. Adopting performance-based payments is one of many approaches used by high-performing companies.
The final important consideration is patient satisfaction, an indicator that has been linked with improved health outcomes and fewer medical malpractice suits. With patient-centeredness in mind, the goal of monitoring patient satisfaction is to improve the care provided through the integration of feedback. Companies that perform relatively well are those that administer a satisfaction survey to patients and incorporate its findings to tailor care delivery.
Implications for Investors
Governments will likely continue to incentivize value-based care, especially in the U.S., a country in which the population is aging, developing chronic diseases, and falling under the poverty line. The conditions mean that in the U.S., the number of Medicare and Medicaid beneficiaries will likely increase and consequently the value of contracts will increase. In turn, the value of payments at risk will also increase, especially if guidelines are not appropriately followed. The increasingly stringent monitoring and oversight from governmental agencies signals the importance of the subject.
Investors may wish to give careful consideration to how managed care companies manage risks related to health outcomes and value-based payments. In particular, investors may wish to consider how these companies assess the health profiles of their enrollees, whether evidence-based AI tools are used to substantiate risk scores (where applicable), the extent to which wellness programs are available and accessible, and/or how performance is being monitored and managed.
Explore ISS ESG solutions mentioned in this report:
- Identify ESG risks and seize investment opportunities with the ISS ESG Corporate Rating.
Authored by:
Stephanie Aboueid, Sector Lead, Healthcare, ISS ESG
Amber Daniels, Sector Head, Healthcare, ISS ESG




